|
Endoscopic Spine Surgery |
|
Introduction
Clear visualization of nervous tissue, the intervertebral disc and other surrounding structures is often the key to success in any decompressive spine procedure.
The process of visualization in the past has meant open surgery with a translaminar access pathway that involves extensive muscle and ligament stripping, muscle and skin retraction, devascularisation, bony resection of normal parts of the spinal canal including lamina resection as well as facet joint ligamentous, capsular and bony violation in order to gain access to within the spinal canal. Once the spinal canal is reached, further exposure requires the need for dural and root retraction with inherent risk of epidural scarring and fibrosis. The size area and magnitude of the surgical wound is disproportionate to the size of the pathology, which is often measure in the magnitude of a few millimeters only. Realizing the above, in the late 1960’s Yasargil described microscopic discectomy utilizing the operating microscope[1]. The size of the surgical access wound had decreased but the problem of surgical trauma to the structures constituting the borders of the spinal canal was more or less the same, with the same need for laminectomy followed by dural and nerve root retraction and the subsequent attendant risk of development of epidural fibrosis and scarring.
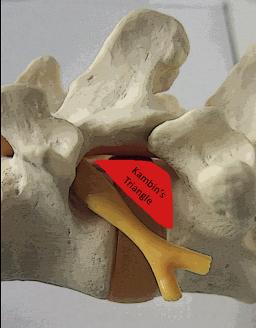
Discal pathology is located ventral to the spinal canal, obviously an access pathway that would not require a translaminar approach with breach of the dorsal column was required. In 1972 Kambin described a posterolateral approach for a limited nucleotomy, defining the safe triangular working zone (Kambin’s triangle), being the site for safe surgical access to the disc through a posterolateral approach (fig.1). |
|
Copyright © 2008 Spine Care Hong Kong |
|
Fig.1
|
|
Hijikata subsequently described percutanous manual discectomy for central nucleotomy[2] in 1975. Other reports were by Kambin and Gellmann[3] in 1983. Onik and Helms[4] described Automated Percutaneous Lumbar Discectomy (APLD) with use of an automated aspiration probe. The use of optics in the form of an endoscope was a breakthrough in visualization and it was Kambin [5] [6] [7] [8] in the early 1990’s who first described Arthroscopic microdiscectomy.
Advantages of the Transforaminal Posterolateral Approach
The main advantages of the transforaminal posterolateral approach to the spine are that the erector spinae muscles are not at all violated, therefore post operatively patients do not have to rehabilitate and retrain their back muscles. Minimal fibrosis around the epidural space results as there is minimal retraction or exposure of unaffected and adjacent neurological structures, the only exposure if any is located at the site of pathology. In the presence of mild instability or spondylolisthesis, a posterolateral transforaminal approach will also have the least collateral damage to the paraspinal and bony elements as compared to an open procedure. The incidence and likelihood of development of post operative instability will be minimized. As a result of the smaller wound there is minimal blood loss and the minimal surgical wound trauma means little pain, the procedure can be accomplished under local anaesthesia.
Disadvantages of the Transforaminal Posterolateral Approach
Where the transforaminal posterolateral approach has its advantages for the decompression of extraforaminal, foraminal and lateral recess pathology and other pathology at the intervertebral disc level, other scenarios where the pathology is located at sites cephalad or caudad to the intervertebral disc level means that this approach is less advantageous as the confines of the approach limit proximal and distal exposure being bound by the confines of Kambin’s triangle. In addition the deeper the pathology i.e. postero-central pathology will also mean that the working channel will have very little degree of freedom, the tip of the working channel will become more and more fixed and focused at a particular point and access will become more and more restricted.
The access portal to the L5/S1 level may be difficult due to the presence of the iliac crest inferiorly, especially in male patients with the narrower pelvis. The trajectory of the working channel and endoscope at L5/S1 will always be oblique.
During placement of the working cannula and during use of manual instruments, radiation in the form of x rays almost certainly is used. Radiation exposure can accumulate especially over the surgeon’s hand, there have been reports linking an increased risk of squamous cell carcinoma of the hand and increased incidence of thyroid carcinoma as a result of occupational exposure to ionizing radiation.
Indications and Contraindications:
An accurate diagnosis of the pathology is the key. Symptoms should be documented and those mainly attributable to nerve root compression are the best candidates. Symptoms of mechanical low back pain and those due to instability are probably best treated via and open procedure for decompression followed by stabilization.
In all cases unless there is motor neurological deficit, a period of 4-6 weeks of conservative treatment is recommended. A trial of a selective nerve root block and or epidural steroid injection may also be tried, this will give useful information as to the source of pain, define and localize the “pain generator.
A diagnosis lateral canal or foraminal stenosis either due to subarticular or far lateral disc prolapse will put this technique to advantage over conventional translaminar approaches. Conversely for many authors where the pathology lies in the central portion of the canal, examples being central canal stenosis or more seriously cauda equina syndrome, then the conventional open translaminar approach would still be the safest and easiest decompression option. In cases requiring instrumentation then again, the posterolateral percutaneous approach may have its limitations, however placement of percutaneous pedicle screws and or transarticular facet screws are an option.
Patient Education and Informed Consent
Patients should understand that they are carefully selected for surgery based on their individual history, physical findings and investigations all correlating with the proposed pathology. They should understand that they have been advised for surgery because they have failed conservative treatment. The option for endoscopic surgery has been selected as this offers the most preferential benefit versus cost ratio. The risks associated with this procedure are similar to traditional procedures, namely infection, nerve root and dural injuries, incomplete decompression, recurrent disc herniation or recurrent stenosis are other concerns. The degenerative process will continue and surgery will not retard this. As with all surgical procedures once the procedure is performed there is no going back. Some bridges will be burned, however because this procedure is truly minimally invasive and percutanous, the amount of bridge burning is considerably less than with more traditional surgical procedures with their associated approach related comorbidities. The endoscopic posterolateral transforaminal approach has little as regards approach related comorbidity and the form of anaesthesia used is usually local anaesthesia or MAC. The usual requirement for general anaesthesia in open procedures is not necessary and it is in fact a disadvantage as the patient will the local anaesthetic will be able to feedback to the surgeon if there is any discomfort, this makes the percutanous endoscopic procedure a relatively safer procedure.
Surgical Planning
The entry trajectory to the affected level may be projected using data obtained from CT or MRI scans that include the imaging of the dorsolateral skin for the proposed entry angle and trajectory. (fig 2.)
|
|
As a rough guideline anywhere from 10 to 15 cm from the midline is a good starting point, this figure must take into consideration facet joint size and morphology, the amount of subcutaneous adipose tissue and the muscularity of the patient. In general a patient with an increased abdominal girth will require a more lateral skin entry site. The proposed trajectory should target the base of the safety triangle ( Kambin’s triangle) as this area offers the greatest margin of safety.
Surgical Technique
The procedure is usually carried out under local anaesthesia. Fluoroscopic imaging is used to assess placement of the needle tip, the needle tip is advanced towards the more caudal part of Kambin’s triangle as this is the base of the triangle and being the widest part and affords the greatest margin of safety.
Subsequently a correctly placed needle tip will be when on simultaneous 2D fluoroscopy on the lateral view the needle tip is at the dorsal edge of the posterior disc annulus on the lateral fluoroscopic view and on the AP view the needle tip is between the mid and medial pedicle lines.(fig. 3 and fig. 4). |
|
Fig. 3 and 4
After confirmation of accurate placement of the needle,a short acting local anaesthetic, such as xylocaine is injected into the area to anaesthetize the lateral aspect of the posterior longitudinal ligament and the posterolateral disc annulus prior to annulotomy.
The stylet of the needle is then replaced by a guide wire and the guide wire is then advanced into the central portion of the disc.
At this stage Indigo Carmine a basic dye is injected into the disc. It will preferentially stain the acidic disc annulus and nucleus, this is a very important as it then will allow easy identification of disc tissue versus other tissues especially neural tissue.
The skin incision is then lengthened to accommodate the soft tissue dilators, this may be a single instrument cannulated orbturator or a set of serial cannulated dilators up to the size of the appropriate working channel or cannula. The dilator obturators and guide wire are removed to leave the cannula in place.
An inflow and outflow irrigation system are connected and the working channel endoscope can then be introduced.
Upon establishment of positive pressure irrigation (usually a gravity feed system) any minor bleeding will be controlled and a clear field can be visualized.
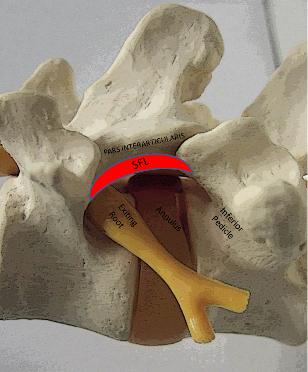
The following structures should be remarked upon before proceding: at superiorly the pars interarticularis and superior foraminal ligament, cephalad and inferiorly the exiting nerve root, caudally the inferior pedicle. Straight ahead will thus be the posterolateral annulus and disc space. (fig.5) |
|
Fig.5
The working cannula should at all times be situated lateral to the medial pedicle line as this represents the lateral extent of the dural sac and traversing nerve root, any medial impingement by the edge of the cannula risks dural laceration.
Decompression should be commenced by first improving visualization of the offending structure and thus being able to assess the relevant pathology in terms of neural compression. Often this may mean resection of overlying and more superficial structures in order to achieve better visualization and achieve more working space.
Bone resection may be achieved by use of endoscopic shavers or lasers, Bleeding may be encountered in the form of epidural venous plexus, this may be addressed by radiofrequency coagulation or laser coagulation.
The disc should now be easily visible as it has been stained by the previously injected indigo carmine dye. Disc material that is dorsal to the vertebral body and PLL is removed, additional removal of any loose fragments or complete fragments will depend on operator preference.
Controversy exists in the amount of disc excision, as in microdiscectomy, the question of how much nucleus pulposus to excise remains. Many operators advocate to try to preserve disc height and stability and excise the herniated portion and hope that the remaining defect will scar and seal off, others faced with the risk or experience of reherniation may advocate to do more and remove the remained of any “unstable” nuclear material. In any case after the discectomy the remaining annulus and posterolateral aspect of the PLL, facets and other structures that may come into contact with the decompressed nerve root should be denervated by radiofrequency ablation or by laser coagulation. This will minimize the onset of or recurrence of discogenic or other forms of pain after the procedure.
Summary
The term minimally invasive surgery encompasses many procedures that achieve their result through a smaller access portal. Whereas in the more traditional approaches such as microdiscectomy are modifications of open laminotomy and other transcanal procedures, endoscopic spine surgery through a posterolateral extracanal approach is a newer and truly canal sparing procedure.
This technique has been made available through parallel development keeping pace with technological advances in fiber-optics materials, instrument and imaging technology.
As new techniques develop, new learning curves will follow. Surgeons used to the open and minimally invasive translaminar approaches will have to familiarize themselves with anatomy from the “other side of the fence”. An intricate knowledge of extraforaminal anatomy and approach together with mastery of new techniques in handing of endoscopic instruments and 3D coordination will result.
References 1. Yasargil MG (1977) Microsurgical operations for herniated lumbar disc. Adv Neurosurg 4:81-82 2. Hijikata S, Yamagishi M, Nakayama T, et al ( 1975) Percutaneous discectomy: a new treatment method for lumbar disc herniation. J Toden Hosp 5:5-13 3. Kambin P, Gellman H ( 1983) Percutanseous lateral discectomy of the lumbar spine: a preliminary report. Clin Orthop 174:127-132 4. Onik G, Helms C, Ginsburg L, et al (1985) Percutaneous lumbar discectomy using a new aspiration probe. AJR Am J Roentgenol 144: 1137-1140 5. Kambin P (1991) Arthroscopic microdiscectomy. Semin Orthop 6:97-108 6. Kambin P (1991) Arthroscopic microdiscectomy: laser nucleolysis. Philadelphia Med 87: 548-549 7. Kambin P (1992) Arthroscopic microdiscectomy: Arthroscopy 8: 287-295 8. Kambin P (1996) Arthroscopic microdiscectomy. In: Frymoyer J, Ducker T, Hadler N, Kostuik J, Weinstein J, Whitecloud T III (eds) The adult spine principles and practice, 2nd edn. Raven, New York |

|
SPINE CARE HONG KONG |
|
ACCURATE DIAGNOSIS, STRUCTURED TREATMENT |